Sidebar Menu
Implementing a Self-measured Blood Pressure (SMPB) Program
Implementing a Self-Measured Blood Pressure (SMBP) program involves several key steps to ensure effectiveness and successful integration into clinical practice. To verify the diagnosis of hypertension or manage a patient’s medication or treatment regimen, it may be helpful to have the patient do blood pressure readings outside of the clinic. Implementing an SMBP program where patients use a home monitoring system can help you get the readings or information you need to make clear clinical decisions regarding hypertension diagnoses and control. There are 4 steps you can take to implement or improve an SMBP program and engage patients in the management of their blood pressure. In each of the 4 steps below there are additional resources to enhance your learning.
Steps:
-
Design and implement an SMBP protocol
-
Ensure standardized procedures and workflows are followed and objectives are clearly established. Determine specific goals, such as improving blood pressure control, empowering patients in self-management, and enhancing communication between patients and providers. Guidelines and protocols for blood pressure management program can help organizations to establish standardized procedures for patient eligibility, monitoring frequency, target ranges, and appropriate actions based on blood pressure readings.
- Create guidelines and protocols that outline the program’s procedures, including patient eligibility criteria, the recommended frequency of blood pressure measurements, target blood pressure ranges, and actions to take based on blood pressure readings.
- Choose validated and accurate blood pressure monitoring devices suitable for home use.
- Assemble a team within the clinic that will support the SMBP program. This is essential for continuity and standardization. Along with clinical staff members such as MA’s or Nurses, include at least 1 provider on the health care team. If multiple providers will participate, designate a provider champion. Having a provider champion provides high-quality care and ensures that care never falls below the standard and will help with clinician buy-in and dissemination of protocols and workflows throughout the clinic.
- Provide staff competency training to ensure each staff member involved in the SMBP process is trained in how to instruct patients to conduct proper home monitoring. Staff blood pressure competency training should be conducted bi-annually or annually. (Consider using the clinical competency guide located in the resources of this section)
- Train all staff on the SMBP program, including its benefits, procedures, and appropriate interpretation of blood pressure measurements. Ensure they understand the role of SMBP in hypertension management and can efficiently communicate with patients about the program.
- Prepare patient education materials regarding SMBP, including proper measurement techniques, appropriate cuff sizing, and monitoring frequency. Ensure patients understand how to accurately record their readings and transmit the data to the clinic.
- Determine the frequency and duration of self-monitoring based on individual patient needs. The patient should measure their blood pressure at home multiple times a day, at different times of the day, for a specified timeframe. Define the timeline that works best for the patient and their follow-up visits to review data.
- Schedule follow-up visits to review the patient’s blood pressure measurements. It is important to note that these are general guidelines, and the exact frequency of follow-up visits should be determined by the healthcare provider, taking into consideration the individual circumstances.
- For patients with well-controlled blood pressure or with no significant underlying health conditions, follow-up visits may be scheduled for 3 to 6 months. This frequency could allow for adequate monitoring and adjustment of medications or lifestyle modifications.
- For patients with hypertension, especially those with more severe or uncontrolled blood pressure, more frequent follow-up visits may be necessary. In such cases, visits every 1 to 3 months may be recommended to closely monitor the patient’s progress and make timely adjustments to the treatment plan.
- Evaluate the data, compare with target ranges, and provide feedback. Use these follow-up visits to adjust treatment plans, lifestyle modifications, and address any questions the patient may have.
- Cultivate effective communication between patients and providers. Encourage your patients to share their blood pressure readings and any concerns they may have. Establish a system with your staff and providers to implement prompt feedback and guidance to support patient self-management.
- Offer ongoing support and resources to patients participating in the SMBP program. This could include educational materials, lifestyle modification guidance, and encouragement.
DEVICE LOANER PROGRAM
Decide if your clinic will be providing loaner devices or asking patients to purchase their own. Consider purchasing a supply of SMBP loaner devices for patients unable or unwilling to purchase a device for themselves. Consider following these steps when setting up your loaner program:
- Assess the demand for blood pressure monitor loaner devices in your practice. Identify patients who may need temporary access to a device, such as those patients who are undergoing evaluation, are experiencing device malfunction, or are awaiting a permanent device. Define the criteria for patients to qualify for a loaner device. This could include medical conditions, insurance coverage, device malfunctions, and any other relevant situations. Make sure the criteria are communicated to patients and providers.
- Purchase a supply of blood pressure monitor loaner devices to meet your identified needs. Ensure these devices are in good working condition and are validated and calibrated.
- Create a loaner device agreement that outlines the terms and conditions for borrowing a device. Include in the agreement information on device responsibilities, return timelines, potential fees for lost or damaged devices, and patient obligations on using, maintaining, and returning the device to the practice.
- Determine which patients may be eligible to receive a discounted monitor through their insurance, such as Medicare, or, if relevant, check with your state to see what coverage exists under Medicaid plans (see link below). Sometimes, commercial insurance carriers will cover the cost of a patient blood pressure monitoring device.
Links:
List of Devices that have been validated
American Medical Association Patient Training Checklist for Loaner Device
American Medical Association Loaner Device Agreement- English
American Medical Association Loaner Device Agreement- Spanish
American Medical Association Loaner Device Inventory Management
NACHC Self Monitoring Blood Pressure Implementation Toolkit
NACHC/Million Hearts Learning Lab Miscellaneous resources including patient training videos
SMBP Monitoring Action Steps for Clinicians
AMA Self-measured blood pressure cuff selection
Competency on Training Patients Self-Monitored Blood Pressure
-
Identify Target Patient Populations
-
Analyze patients with elevated blood pressure readings to determine if monitoring at home will help identify/confirm hypertension or aid in treatment intensification using medications or other dietary changes. Train the patient to use the BP monitor and assess their ability to use the blood pressure device as well as their health and digital literacy levels to ensure understanding.
Potential candidates for SMBP might include::
- Patients newly diagnosed with hypertension
- Patients with potential undiagnosed hypertension
- Patients with medication adherence challenges
- Patients who are unable to travel to the office to be measured
- Patients who have the digital and health literacy to comply with measurement and reporting requirements
Links:
NACHC SMBP Implementation Guide
Million Hearts SMBP Guide for Clinicians
American Heart Association patient education and resources for SMBP
-
Train patients on proper home blood pressure measurement techniques
-
Training patients to follow established blood pressure measurement techniques is vital for accurate results and effective use of SMBP to support hypertension management. Like staff training, it is important that patients understand proper techniques and positioning for accurate blood pressure measurement.
Here are the steps to train patients in this process:
- Explain to the patient the significance of home blood pressure monitoring in managing their hypertension.
- Assist the patient in choosing a validated and accurate blood pressure device. Help with recommendations on reliable models.
- Advise the patient to carefully read and understand the user manual that comes with the device.
- Instruct the patient on proper positioning and cuff placement.
- Ask the patient to demonstrate how to take their blood pressure with the device.
- Encourage the patient to take measurements at different times of the day. Explain to the patient that providing multiple readings allows the provider to average those readings for a more accurate representation of their blood pressure.
- Schedule regular follow-up visits to review the patient’s home blood pressure measurements. Assess their progress, address any questions, or adjust treatment plans if necessary.
Links:
Checklist for staff when training patient during an in-person encounter
Checklist for staff when training patients during virtual encounter
American Medical Association Self Measure Blood Pressure: Seven day recording log
American Medical Association Patient education handout describing SMBP
American Medical Association Patient Education Infographic on proper positioning for SMBP- ENGLISH
American Medical Association Patient Education Infographic on proper positioning for SMBP- SPANISH
American Medical Association SMBP Training video for patients
-
Enroll patients in the Self-Measured Blood Pressure (SMBP) program
-
Patients will need to report readings at an established frequency. Make sure that patients are aware of when and how to report their readings, then collect their data and interpret the results.
1. Collecting data
While digital transmission direct from device to the EHR is preferred, ask the patients to return their readings log in the way that works best for them. (i.e., Phone call, Notebook, or Spreadsheet) Most important is that the patient is taking and reporting readings.
2. Interpreting results
When a healthcare provider wants to average multiple blood pressure readings, consider these steps:
- Collect Multiple Readings: The patient is usually instructed to take several blood pressure measurements over a period of time. This can be done at home using a home blood pressure monitor or during visits to the office.
- Record the Readings: The patient records each blood pressure reading, along with the date and time of measurement. This information is important for tracking trends and identifying any significant changes.
- Exclude Outliers: If there are any readings that appear to be outliers, such as extremely high or low values that are inconsistent with the patient’s typical blood pressure range. The provider may exclude them from the averaging process. This is done to ensure that unusual readings don’t skew the average.
- Calculate the Average: Once an appropriate set of blood pressure readings is obtained, the healthcare provider adds them together and divides the sum by the number of readings to calculate the average. For example: if there were five readings (120/80, 122/78, 118/82, 124/76, 120/80), the average would be (120 + 122 + 118 + 124 + 120) divided by 5=604 divided by 5=120.8/80.8.
- Interpret the average: The average blood pressure value provides a more reliable representation of the patient’s overall blood pressure status compared to individual readings. It helps the provider assess the patient’s blood pressure control, monitor any changes over time, and make informed decisions regarding treatment or adjustments to the management plan.
It is important to note that healthcare providers may have their own protocols or variations in the way they calculate averages, a general principle is to sum up the readings and divide by the total number of readings to obtain the average blood pressure value.
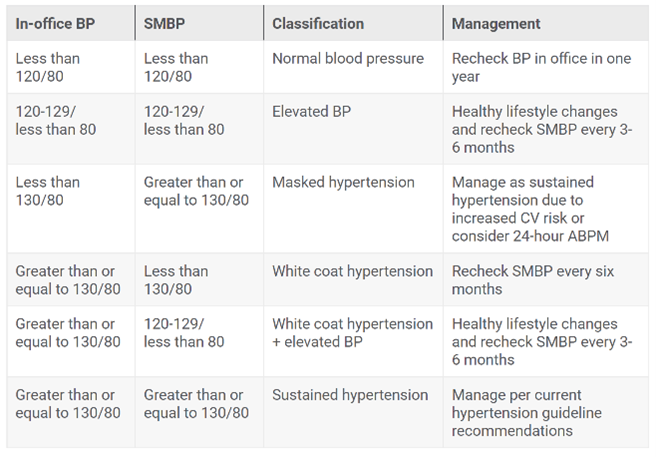
Use this chart to reconcile in-office BP and SMBP measurements to classify and manage patients.
Links:
American Medical Association Target: BP Data collection guide
American Medical Association 7-Step SMBP Quick Guide for Clinics
American Medical Association Blood Pressure Interpretation Tables
